Choosing the Right Surgical and Exam Gloves
Disposable gloves are one of the highest volume supplies for hospitals. With various departments, clinical tasks and all member of staff requiring different types and sizes of gloves, choosing the right one can be challenging.
Thanks to advancements in technology, exam and surgical gloves today have more features and benefits than ever before. Medline wants to make it easier for you to evaluate all the options on the market in order to select the right glove and material.
This guide breaks down the differences between major glove types in order to educate and help you make informed decisions.
Why Use Accelerator-Free Gloves?
A high percentage of healthcare professionals suffer from glove-related hand allergies. Clinical evidence shows that over 80 per cent of allergic contact dermatitis is attributed to a chemical allergy.¹
A chemical allergy is a reaction to specific allergens such as chemical accelerators used in the glove manufacturing process of both latex and synthetic gloves.² Using an accelerator-free glove can help prevent a user from suffering an outbreak.
Gloves with Accelerators Can Cause Chemical Allergies
Clinically speaking a chemical allergy will present itself as red, irritated, cracked and itchy skin on and around the area of contact.
The chemical allergy response begins when the antigens, such as residual chemical accelerators, leach from the glove and penetrate the skin, triggering the formation of T cells sensitised to the specific antigens.
Repeated exposure to the antigen in individuals who are allergic results in the reactivation of sensitised T cells and incites the inflammatory response causing the symptoms of red and itchy skin.²
How to Prevent Chemical Allergies
There are many ways to identify a chemical allergy, such as patch testing, diagnostic skin testing and blood or allergy testing. Once the chemical allergy is determined as the cause, the primary treatment is avoidance or minimisation of exposure to the allergen; however, there are also some medications and moisturisers that can help alleviate the symptoms.
DID YOU KNOW?
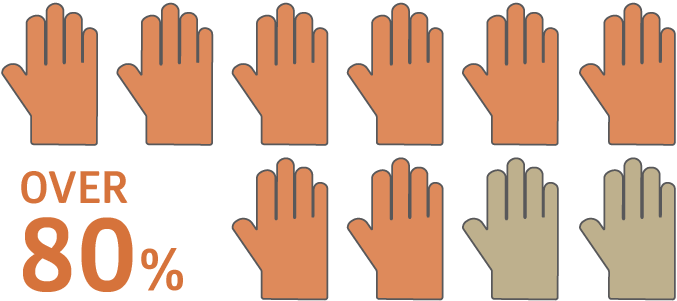
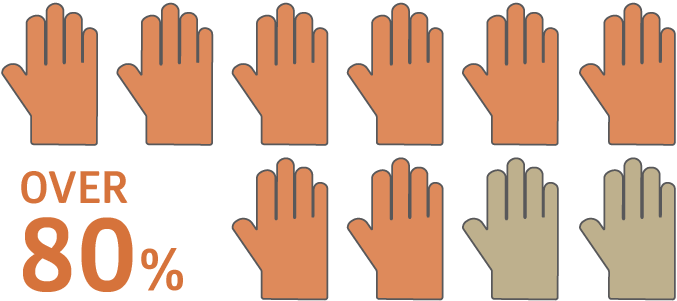
of reported glove-associated allergic contact dermatitis is attributed to chemical accelerators.⁵


of 954 respondents at AORN congress indicated that staff continued to have allergy issues even when they switched to gloves without natural rubber latex.⁹
What Are the Different Types of Accelerators?
Accelerators are the chemicals used in the glove manufacturing process to help make gloves more durable and elastic. Some of the common chemical accelerators used are thiurams, dithiocarbamates, mercaptobenzothiazoles and diphenylguanidine.
Chemical
Reaction
Role in Glove Munufacturing
Thiurams
Account for 60% of accelerator-related skin irritation and are the primary cause of chemical allergy.³
The universal vulcanising agent for rubber is sulphur. Thiurams are ultra-fast accelerators and are the preferred primary accelerator for sulphur-cured rubbers with low unsaturation content. Thiurams are used as vulcanising agents in the absence of sulphur; the vulcanisates attain high degree of state of cure, exhibiting high tensile strength, lower elongation at break, higher rebound resilience and lower tear resistance.3 Because manufacturers can produce gloves containing thiurams in high quantities, the overall cost is low.
Dithiocarbamates / Carbamates
Account for 30% of accelerator-related skin irritation.³
Dithiocarbamate accelerators are widely used as ultra-fast accelerators for natural rubber latex-based compounds that absorb sulphur and facilitate cross-linking. They can also find applications as primary or secondary accelerators in most dry rubber-based sulphur-cured compounds.⁴
Mercaptobenzothiazoles (MBTs)
Account for between 1% and 5% of accelerator-related skin irritation.³
MBTs are a fast curing accelerator suitable for most common rubbers and contribute to tensile strength; the presence of stearic acid and zinc oxide is necessary for good cures. MBTs cause fewer cases of contact sensitivity.⁴
Diphenylguanidine (DPG)
Allergic reactions to this chemical are on the rise according to some recent reports.³
Diphenylguanidine is used as a secondary foam stabiliser in the silicofluoride foam process. It does not show better activity than thiuram and dithiocarbamates, but it does have better stability and also contributes to tensile strength. It is used as a complexing agent for the detection of metals and organic bases.⁵
Accelerator-Free Gloves
Accelerator-free gloves are a solution to the growing number of cases of type IV allergies.6 They will help reduce the number of professionals suffering from skin irritation not caused by latex. With a variety of options on the market, switching to accelerator-free gloves will allow individuals who have chemical allergies to continue working safely. It will also lessen treatment costs and limit the use of external staff when regular staff are unable to work.
The Next Evolution in Surgical Gloves


1947
First surgical gloves to contain powder, natural rubber latex and chemical accelerators


1983
First powder-free surgical glove but still contains natural rubber latex and chemical accelerators


1990s
First surgical glove not made with powder and natural rubber latex, but still contains accelerators
2016
Medline introduces next-generation surgical glove not made with powder, natural rubber latex and chemical accelerators
Why Use Latex-Free Gloves?
There are multiple benefits to using latex-free gloves, for patients and staff as well as medical centres and the broader healthcare industry. Latex can cause varying degrees of allergic reactions, ranging from a stuffy nose and asthma attacks to anaphylaxis and very rarely, death.¹ Some groups of society are especially susceptible, so it makes sense to use latex-free gloves across all health centres, thus eliminating the risk altogether.
Allergy Assessment
Whilst skin prick tests are available to assess sensitivity, these are costly and time-consuming.
Many patients and staff are unaware of their latex allergy, so this makes effective risk assessments difficult to perform.
With this in mind, healthcare professionals may choose to use latex-free gloves as a precautionary measure, particularly because it is fairly common for latex allergies to build up over time or develop suddenly and unexpectedly.¹
Hospital Impact
Every time there is an incident involving latex gloves, it affects health, productivity and finances. Healthcare workers who have a latex allergy may have to deal regularly with dry, itchy and irritated skin; this could cause them to miss work because their hands are in such poor condition they cannot wear gloves.
When the regular staff is absent, temporary or external staff need to fill in. This could slow down hospital productivity and efficacy because they are not as familiar with the rounds, patients or policies.
From a financial point of view, the use of latex gloves could cost the hospital more money for treatments and creams for those effected by the allergy and increase the wage bills to external agencies.
The COVID-19 pandemic has resulted in significant challenges within the healthcare sector, including surgical backlogs, heightened healthcare costs, and a shortage of staff.
During the pandemic, 21 per cent—now 18 per cent—of persons needing care in the European Union could not access medical examinations or receive treatment because clinical teams were overstretched, and preliminary assessments prioritised certain care services,¹⁹ and unfortunately, this trend does not show signs of ending in the short term.
Addressing the staff shortage, the European Commission estimates that an additional 1 million nurses are required to meet current healthcare demands. Furthermore, the financial strain on healthcare facilities has been substantial since the onset of COVID-19. Hospital labour expenses have surged by more than one-third compared to pre-pandemic levels.²⁰
By using only latex-free gloves, the cost of stock may decrease, as buying one product in bulk tends to be cheaper than purchasing multiple products. Additionally, the number of incidents occurring in latex-free wards, for example, decreased dramatically when an immediate swap to latex-free gloves was enacted.³ Reducing the number of incidents will directly correlate with lowered treatment costs for latex-induced allergic reactions and decrease the costs related to sourcing temporary or external staff.
Using latex-free gloves is not only cost-effective, but also clinically responsible and time-saving. Making the change to latex-free gloves can allow patients to feel confident and secure throughout treatment, as well as contribute to a smooth-running healthcare facility. As these are all priorities for healthcare professionals, taking advantage of opportunities to make a difference is in alignment.
The hidden costs of using latex
Here is an overview of what hidden costs could look like when latex-based gloves are used:
Direct
- Latex allergy disability compensation (HCW)
- Latex allergy single event compensation (HCW)
- Latex allergy compensation in case of disability/death (Patients)
- Latex allergy defense costs (HCW)
- Latex-related medical care
- Sick leave replacement
- Cancelled or delayed surgery for latex-sensitive patients
- Latex supply replacement
Indirect
- Diagnostic tests to determine sensitivity
- In- service training for staff
- Time for developing policies and procedures
Incalculable
- Decreased staff productivity
- Decreased procedures quality
- Patients and workers’ satisfaction
To go even further in our support, we have built a tool that is intended to simulate the potential hidden costs of latex-based surgical glove usage in your facility. Medline’s ‘Hidden Cost Calculator’ can help you explore the idea of moving towards latex-free surgical gloves by facilitating your understanding of the estimated risks of using latex-based gloves when treating patients and healthcare professionals.
Why Use Powder-Free Surgical Gloves?
The use of powdered gloves remains prevalent in hospitals and surgeries, despite the wide range of risks and multiple international organisations advocating a switch to non-powdered stock. This means that preventable situations are occurring with both patients and staff.
Multiple studies have been conducted around the world and they have revealed a number of concerns. In some countries these studies have resulted in an outright ban of powdered gloves. There is wide-ranging literature supporting and explaining how changes can be made. The FDA (US Food and Drug Administration) has already banned the use of all powdered gloves.1 In the UK, there are government-led and health authority recommendations in place to discourage the use of powdered gloves.2
Staff Safety
The health of staff is directly connected to smoothly running hospitals. Infection control is understandably a key aspect of patient care, which should be prioritised, but perhaps other issues such as allergic reactions are not as widely understood.
Asthma and other breathing problems are connected to the use of powdered gloves because of the potential airborne nature of the powder. Conjunctivitis and joint inflammation are also most commonly connected to the use of powdered gloves.3
Dry skin, which can be exacerbated or turn into Irritant Contact Dermatitis (ICD),4 becomes difficult to manage and treat if powdered gloves continue to be used by healthcare professionals.
Prevention of Germ Transmission
Concerns around the use of powdered gloves are common in regard to wound closure too. The issue here is simply that any tape used to close a wound is more likely to stick to a powdered glove than a non-powdered one worn by the physician.
The powder that coats the gloves binds with sweat and any mucous and this contributes considerably to the risk of infection being spread across clinical spaces. As the powder comes into contact with equipment and fittings, infection or germs can begin to spread and are hard to isolate. More chemicals are contained in and are used for making powdered gloves. These chemicals can cause an allergic reaction and also make it harder for existing conditions to heal. This impacts the clinician’s ability to carry out frontline duties of care, which in turn may contribute to staff shortages and related cost issues, such as having to pay for external agency staff.
The smooth running of clinical spaces means meeting the needs of patients and staff in cost-effective and efficient ways. The challenge of providing a safe barrier against dirt and infection can be successfully overcome, as can ensuring that allergic reactions are kept to an absolute minimum, but investment and the openness for change are necessary. Non-powdered gloves are a sure way of impacting both of these challenges with instant and far-reaching results.5
Why Double Glove?
The risk of exposure to blood-borne pathogens is a major concern for surgeons and operating theatre staff. Although often undetectable to the human eye, microperforations in surgical gloves are large enough to allow pathogens to pass between the glove wearer and the patient and cause infection.
A recent study reported that over 80 per cent of all surgical glove perforations go unnoticed.¹ Another study reported that the incidence of glove microperforations increased with duration of wear.²
A proven method to reduce these risks is to double glove with a dark-coloured underglove.
Double Gloving Technique
While wearing a single glove protects the wearer from blood-borne infections, more protection is needed when needles and sharp instruments are involved, due to the high risk of punctures. Wearing two pairs of surgical gloves greatly minimises the risk of cross-contamination by adding an extra layer of protection.
VIDEO
Double Gloving Technique
If a perforation occurs, the inner glove is protected by the outer glove. A study by the American College of Surgeons showed double gloving reduces the risk of exposure to patient's blood by as much as 87 per cent when the outer glove is punctured.³
With the double gloving technique, the number of perforations in the inner glove can be reduced significantly, and the surgeon can identify holes faster when a darker underglove is used. According to a clinical study in the AORN Journal, when using on underglove with a contrasting colour, 84 per cent of perforations were recognised in an average of 22 seconds, whereas 8 per cent of perforations were identified in 47 seconds when using a single glove.4
How Does the System Work?
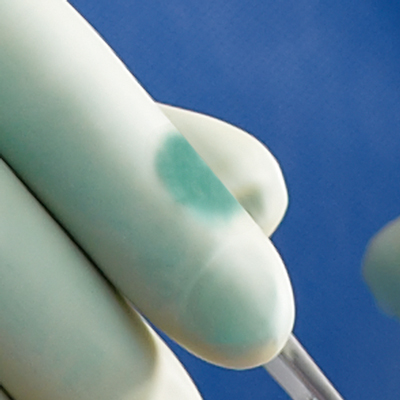
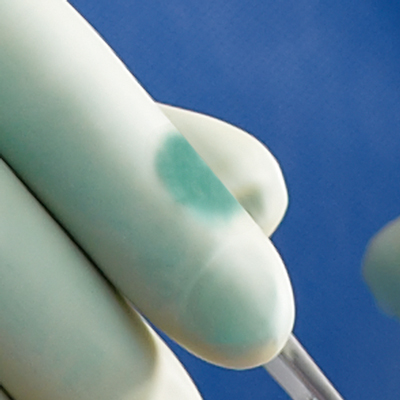
The wearer dons the specially designed darker-coloured underglove as the first layer of protection followed by a light-coloured or translucent overglove.
In the event that the outer glove is breached during surgery, blood and other fluids seep between the two glove layers, and the contrasting colour of the dark green underglove alerts the wearer to change gloves.
Changing gloves immediately following the breach minimises the risk of transmission of pathogens between the wearer and the patient.
While double gloving combinations are often a personal preference, it is highly recommended to use a different coloured underglove in order to spot the breach more quickly if the glove is punctured.
What About Surgical Technique?
Many surgeons are reluctant to use the double gloving technique because they feel it may reduce their tactile sensation and, consequently their dexterity can be impaired. However, a study conducted by the Royal College of Surgeons of England on double gloving and surgical technique shows that there is no significant difference in the surgical technique when using single gloves or double gloves.5 The results suggest that double gloving does not alter the surgeon's dexterity.
References
¹Edlich R, Wind T, Hill L, Thacker J 2005 Resistance of double glove hole puncture indication systems to surgical needle puncture Journal of Long-term Effects of Medical Implants 15(2) 85-90
² Partecke, Lars Ivo, Anna-Maria Goerdt, Inga Langner, Bernd Jaeger, Ojan Assadian, Claus-Dieter Heidecke, Axel Kramer and Nils-Olaf Huebner. 'Incidence of microperforation for Surgical Gloves Depends on Duration of Wear.' Infection Control and Hospital Epidemiology 30.5 (2009): 409-14. Print
³ Berguer R & Heller PJ. Preventing sharps injuries in the operating room. Journal of the American College of Surgeons. 2004; (199)3:462-467
⁴ Thomas-Copeland, Do Surgical Personnel Really Need to Double-Glove? AORN Journal, FEBRUARY 2009, VOL 89, NO 2; page 327. 5. Korniewicz D & El-Masri M. Exploring the benefits of double gloving during surgery. AORN Journal. 2012; 95(3):328-336
⁵ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2497939/
⁶ Part 1, Pages 831 – 839. Available at: www.jaad.org Accessed 17 December 2015.
⁷ https://www.henryschein.com/us-es/images/medical/PPE-Chemical-Allergy-Masquerade.pdf
⁸ http://latexallergyresources.org/sites/default/files/newsletter-attachments/The%20ALERT%20May%202012.pdf
⁹ http://www.nocil.com/Downloadfile/DTechnicalNote-Vulcanization-Dec10.pdf
¹⁰ http://www.chemicalland21.com/specialtychem/perchem/DIPHENYL%20GUANIDINE.html
¹¹ Gardner N. Accelerator free fact or fiction. Health & Safety International. October 2008. Available at: www.shieldscientific.com Accessed December 17, 2015.
¹² http://acaai.org/allergies/types/skin-allergies/latex-allergy
¹³ http://www.hse.gov.uk/skin/employ/latex-gloves.html
¹⁴ http://www.safety.admin.cam.ac.uk/files/hsd034c.pdf
¹⁵ https://www.asco.org/advocacy-policy/asco-in-action/FDA-bans-medical-powdered-gloves
¹⁶ https://www.anaphylaxis.org.uk/wp-content/uploads/2016/08/Latex-2016-version-8-with-final-amendment-AS-comms-approval.pdf
¹⁷ http://www.nhs.uk/Conditions/Eczema-(contact-dermatitis)/Pages/Introduction.aspx
¹⁸ http://www.profahandisafe.com/wp-content/uploads/2016/08/Sempermed-Informs-Change-to-powder-free.pdf
¹⁹ Van Ginneken, E., Siciliani, L., Reed, S. E., Tille, F., & Zapata, T. (2022). Addressing backlogs and managing waiting lists during and beyond the covid-19 pandemic. Eurohealth, 35-40.
²⁰ Kaufman, H. (2022). A Special Workforce Edition of the National Hospital Flash Report.
Related Products


